March 6, 2023
Chiquita Brooks LaSure
Administrator, Centers for Medicare & Medicaid Services
Department of Health and Human Services
Hubert H. Humphrey Building 200 Independence Avenue, SW
Washington, DC 20201
Submitted via: https://www.regulations.gov/commenton/CMS-2023-0010-0001
Re: Advance Notice of Methodological Changes for Calendar Year (CY) 2024 for Medicare Advantage (MA) Capitation Rates and Part C and Part D Payment Policies
Dear Administrator Brooks LaSure:
America’s Physician Groups (APG) appreciates the opportunity to respond to the Centers for Medicare & Medicaid Services (CMS) Advance Notice for the Medicare Advantage and Part D programs. We welcome the agency’s openness to stakeholder input and its ongoing commitment to improving health care for all Americans.
Below, APG will first provide (I) a brief description of our organization, followed by (II) a summary of CMS’s proposals, and then (III) our fuller comments and recommendations. Together they reflect the voice of our membership and our commitment to working with the agency to ensure that all Americans have consistently accessible, high-quality, person-centered health care; that health care be equitable; and that the health-care system more fully embrace value-based care models in which providers are accountable for both the costs and quality of care.
I. About America’s Physician Groups
APG is a national association representing more than 360 physician groups that are committed to the transition to value, and that engage in the full spectrum of alternative payment models and Medicare Advantage (MA). APG members collectively employ or contract with approximately 195,000 physicians (as well as many nurse practitioners, physician assistants, and other clinicians), and care for roughly 90 million patients, including roughly 30 percent of all Medicare beneficiaries who are enrolled in MA.
Our motto, “Taking Responsibility for America’s Health,” underscores our members’ preference for being in risk-based, accountable, and responsible relationships with all payers, including MA health plans, rather than being paid by plans on a fee-for-service basis. Delegation of risk from payers to providers creates the optimal incentives for our groups to provide integrated, coordinated care; make investments in innovations in care delivery; advance health equity; and manage our populations of patients in more constructive ways than if our members were merely compensated for the units of service that they provide. Several of our groups do have these delegated relationships with MA plans, while still others – despite their preference for delegated relationships – are in contractual relationships with plans in which they are paid on a fee-for-service basis. In either case, payment-related actions that affect MA plans will directly affect APG providers and their ability to provide optimal care to MA enrollees.
II. CMS’ Advance Notice and Fact Sheet
In its Advance Notice, CMS proposes changes to various aspects of MA payment policies that the agency expects will result in a net increase in revenue of 1.03 percent on average across MA plans. CMS’s estimates reflect an average across MA plans, but individual plans’ experience will vary in a wide range around this average, based in part on the demographic makeup and health conditions of the populations they enroll. Similarly, APG members’ experience will vary depending on the makeup of their patient populations enrolled in MA.
CMS has shared estimates of the effects on MA plans directly with these plans but has not publicly released information about the distribution among MA plans of their expected average change in revenue. Neither has CMS provided information about how the average expected change in revenue will affect different provider groups – including APG members – that contract with MA plans.
CMS’s estimate of the average expected change in MA plan revenue is the net estimated result of updates and changes to various aspects of MA payment policy, such as Star Ratings and benchmark growth rates. There is one aspect that is of particular concern for APG members, as detailed below: CMS’s proposed revisions to the Hierarchical Condition Categories (HCC) risk adjustment model. CMS expects that the agency’s proposed revision of the CMS-HCC risk adjustment model, combined with normalization (a factor that is applied to effectively keep the average risk score at 1.0 in the payment year for beneficiaries in fee-for-service Medicare) will result in a 3.12 percent reduction in risk scores on average across MA plans. CMS also projects a “risk score trend” that CMS expects will contribute to a 3.30 percent increase on average across MA plans.
In addition, CMS proposes to establish a new “Universal Foundation” to align quality measures across MA and other programs. The Universal Foundation would include a core group of measures in the domains of wellness and prevention, chronic conditions, behavioral health, seamless care coordination, person-centered care, and equity. In addition to these shared measures, CMS would continue to apply measures unique to MA and other programs.
Of all these proposed changes, those in the risk adjustment model changes will pose the greatest difficulty for several APG member organizations, as well as contravene important policy directions for the federal government: increasing health equity, boosting primary care, and accelerating the transition from fee-for-service to value-based health care. As detailed below, although the effects differ among APG member groups, many have analyzed the effect on their operations and concluded that they will result in revenue losses that range as high as 17 percent, and possibly higher.
The net effect of these revenue losses will be felt by the patients whom our affected groups serve, who are frequently low-income, racially, and ethnically diverse, and chronically ill. As detailed below, APG believes that there will be particularly negative effects on its member groups that provide mainly primary care – contravening CMS’s other attempts to address primary care shortages and create a more robust primary care sector by boosting payments to primary care practices. The overall result will be poorer care and greater inequities in care, rather than the increased equity and greater quality that CMS seeks. An additional result may be to force APG member organization groups out of these delegated relationships with health plans in which they assume direct accountability for costs and quality – thwarting CMS’s goal of ensuring that all Medicare enrollees have these accountable relationships with their providers by 2030.
Because APG believes these likely effects were unintended consequences of CMS’s proposed changes, APG asks that the agency put the changes on hold for a year to carry out further study and discussion with stakeholder groups. Changes in the risk adjustment model are long overdue, and APG fully supports a holistic set of reforms to ensure that payment is appropriately tailored to Medicare beneficiaries’ underlying demographics and health needs while also maintaining the integrity of the Medicare program. However, it is not appropriate to undertake such sweeping changes as are now proposed on a short-turnaround basis. Below, APG advances other recommendations for approaching these fundamental issues in MA in a more rational and thoughtful way that will complement CMS’s goals of greater equity and speeding the transition to value.
III. Summary of APG’s Recommendations
A. Recommendations Related to Risk Adjustment Model Revisions
Given the severity of the impact of the proposed risk model revisions, the limited time in which CMS must consider and implement changes ahead of the April 3, 2023, final rate announcement deadline, and our uncertainty about which may prove to be an acceptable approach, APG makes a three-part recommendation in order of preference.
• Recommendation #1: APG proposes that CMS postpone for one year the implementation of the proposed clinical revisions to the risk adjustment model that include changes to diagnosis codes and HCCs. Such a postponement would allow time for the agency to study the variation in impact across groups that contract with MA plans, to share more details about the proposed changes, and to solicit stakeholder input on concerns, data on real-world impacts, and ideas for potential modifications to proposed revisions.
• Recommendation #2: If CMS opts not to postpone implementation of the proposed risk model revisions, then APG proposes that CMS eliminate or revise the proposed changes to the limited number of diagnoses (approximately 20) that result in the largest share of the negative impact.
• Recommendation #3: If CMS rejects the first and second recommendations, then APG proposes that CMS phase in the proposed clinical revisions to the risk adjustment model over two to three years.
B. Recommendations Related to Changes in Part C Star Ratings and a “Universal Foundation” for Potential Future Quality Measures
• Recommendation #1: CMS should weigh carefully whether proposed risk adjustment model changes will conflict with, and even defeat, proposed Star Ratings changes. Having the time to examine the possible interactions among these changes is another reason to postpone adoption of the risk model changes proposed in the Advance Notice.
• Recommendation #2: APG proposes that CMS include a Star Ratings measure to reward MA plans that offer beneficiaries access to physician groups that offer value-based care and are fully accountable for the costs and quality of patients’ care.
IV. APG’s Detailed Comments and Recommendations
A. Risk Adjustment Model Revisions
In its Advance Notice, CMS proposes revisions to the CMS-HCC risk adjustment model including “constraints and the removal of several HCCs in order to reduce the impact on risk scores of MA coding variation from FFS.” The proposed version 28 (v28) would replace the current version (v24) of the HCC model. It would also significantly expand the number of condition categories; constrain the coefficients for certain HCCs to be equal; change the coefficients for multiple HCCs; remove many diagnoses from the model; and remap diagnoses to most of the condition categories. These proposed changes add up to a major update to the CMS-HCC model, which CMS typically undertakes every several years in addition to the annual technical changes that the agency makes on a regular basis.
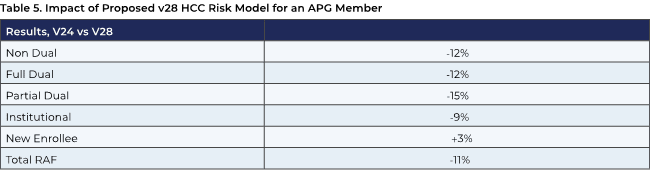
CMS expects that the impact of the agency’s proposed revision to the risk adjustment model will reduce risk scores and their contribution to revenue by a negative 3.12 percent on average across MA plans. The impact for some physician groups that contract with MA plans, including those that are primary care-focused, serve a larger share of disadvantaged Medicare beneficiaries, and embrace value-based care, will be much greater – ranging as much as 17 percent, as noted above. Based on analyses that some APG members have completed, the revenue losses will hit hardest on those organizations that focus their efforts on caring for Medicare Advantage enrollees of low socioeconomic status; who are racially and ethnically diverse; and who have multiple chronic conditions and comorbidities, including diabetes, depression, and cardiovascular disease. Tables 4-5 below, plus several descriptive paragraphs, summarize the anticipated effect of changes for four APG member groups.
Given the scale of the impact for physician groups, APG was disappointed that the description and methodology for CMS’s proposed changes are limited to fewer than 15 pages in the Advance Notice. CMS’s proposal raises many questions that this brevity has left unanswered. At the same time, elements of the description and methodology for CMS’s proposed changes that are included in the Advance Notice raise significant concerns.
CMS indicates that the agency “conducted an assessment on conditions that are coded more frequently in MA relative to FFS” that the agency feels is consistent with “Principle 10” (see below) from a 2000 report in which the authors concluded that risk models should follow ten principles.
Principle 10 -Discretionary diagnostic categories should be excluded from payment models. Diagnoses that are particularly subject to intentional or unintentional discretionary coding variation or inappropriate coding by health plans/providers, or that are not clinically or empirically credible as cost predictors, should not increase cost predictions. Excluding these diagnoses reduces the sensitivity of the model to coding variation and coding proliferation.
The Advance Notice description does not indicate the extent to which the agency weighed the tenth principle (which the authors applied to prospective risk adjustment models) against the other nine. Among the principles that CMS appears to have disregarded, or at least de-prioritized, are the second one – “Diagnostic categories should predict medical expenditures;” the fifth one – “The diagnostic classification should encourage specific coding;” and the seventh one – “Providers should not be penalized for recording additional diagnoses.”
APG takes significant issue with the core underlying premise of CMS’s assessment. It is illogical to compare the diagnoses that are recorded in MA with those that are recorded in FFS. The motivation to record diagnoses is completely different in both programs. That difference does not mean that the diagnoses that are recorded in MA are wrong and that the ones recorded in FFS are correct. In fact, given the lack of incentive in the FFS program, it is more likely that the opposite is true – that MA diagnoses provide a far more accurate reflection of the underlying health status of Medicare beneficiaries.
APG recognizes that there are “wrong” diagnoses included in both MA and FFS and that, given the different incentives, there is a greater risk of “wrong” codes in MA. However, CMS already has an appropriate tool at its disposal for detecting these coding errors: the Risk Adjustment Data Validation (RADV) audits. RADV audits allow the agency to determine which MA plans submit excessive diagnoses, alert these plans to needed corrections if these codes were mistakenly submitted in good faith, and recover misspent funds when codes were fraudulently reported.
In choosing to address what the agency perceives as excessive coding difference between MA and FFS through the proposed clinical revisions to the risk adjustment model rather than through RADV audits, the agency is shifting the greatest weight of the impact away from potential “bad actor” MA plans and onto certain Medicare beneficiaries and the physicians and other clinicians who care for them. The proposed revisions undercut the original reason for risk adjustment: to capture the expected cost to care for a beneficiary so that MA plans (and others) would not face a disincentive to enroll older and sicker beneficiaries.
A tenet of other aspects of health policy holds that “money should follow the person.” By this logic, the risk adjustment model should help to ensure that appropriate payment is linked directly to providing beneficiaries with the care that will address their specific needs. Although it may seem awkward to link human beings to dollar amounts, risk-adjusted payments ensure that plans and physicians have the resources needed to provide care to manage individuals’ chronic conditions and prevent undesirable outcomes, including repeat hospitalizations that further undermine their health. Risk-adjusted payments fund such aspects of care as regular diabetic foot checks, nutritious food to fit strict dietary standards, mental health evaluations and support, and other services that would be unaffordable without this financial support.
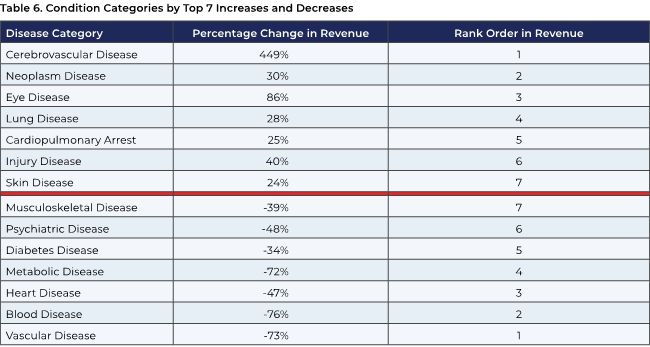
But given analyses completed so far, under CMS’s proposed v28 risk model, money determined by risk adjustment will follow some people much less than others. People with certain chronic conditions, such as diabetes, vascular disease, heart disease, and depression, that are present to a much greater degree among racially and ethnically diverse populations, will bring far less risk-adjusted payment to MA plans and physician groups than is the case under the current risk model.
To illustrate this point, APG commissioned an analysis by ATI Advisory that examined diagnoses across a sample of Medicare beneficiaries in the traditional fee-for-service program. This population was chosen for this analysis because detailed demographic and other information was available (e.g., age, race, ethnicity, limited English proficiency, income relative to the federal poverty line, and food insecurity) along with claims data on utilization, and because examining an FFS population negates any perceived effects from incentives for greater coding inherent in Medicare Advantage. Due to the comment period time constraint, the analysis is limited to select conditions that are significantly impacted by CMS’s proposed revisions: diabetes, heart disease, musculoskeletal, psychiatric, vascular, and kidney.
The ATI analysis shows that the impact of the proposed rule will vary widely depending on patients’ diagnoses (see Table 1 below). For example, two-thirds of Medicare beneficiaries with diabetes would see the adjustment coefficient (i.e., weighting) for related codes decrease, while most heart disease adjustment coefficients would increase. Beneficiaries with psychiatric diagnoses, particularly depression, would be similarly affected, both because of the elimination of codes and decreased coefficients or weighting.
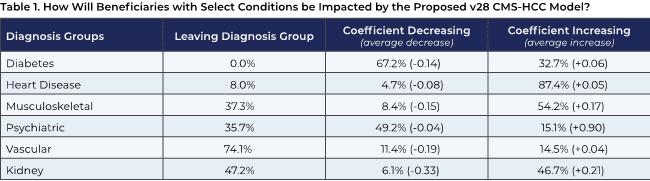 Source: ATI Advisory analysis of 2018–2020 Medicare Current Beneficiary Survey (MCBS) data
Source: ATI Advisory analysis of 2018–2020 Medicare Current Beneficiary Survey (MCBS) data
Based on ATI’s analysis (see Table 2 below) it is likely that the effects of these diabetes risk code coefficient reductions will be disproportionally greater on beneficiaries who are Black and Hispanic or Latino; fully or partially dual eligible; have incomes under 100 percent or 200 percent of the federal poverty level; lack a high school diploma; and are food insecure. Conversely, diabetes codes that will increase will benefit women and those with a college degree more than other beneficiaries.
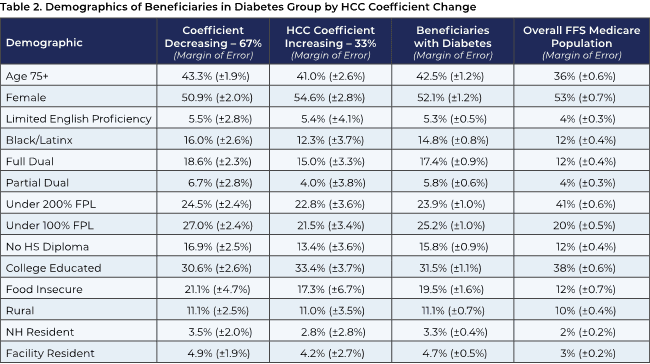 Note: FPL (federal poverty line). Minimal beneficiaries left the diabetes diagnosis group and are excluded from this table.
Note: FPL (federal poverty line). Minimal beneficiaries left the diabetes diagnosis group and are excluded from this table.
Source: ATI Advisory analysis of 2018–2020 Medicare Current Beneficiary Survey (MCBS) data.
The ATI analysis shows differential effects across demographic groups from coding changes in other condition categories, with potentially greater or lesser effects on subpopulations depending on the condition. For example, decreasing the HCC coefficients or eliminating codes for musculoskeletal conditions will have a potentially large effect on women, who make up more than half of the overall Medicare fee-for-service population (see Appendix). By contrast, a substantial increase in coefficients (weighting) for heart disease may have a largely neutral effect on this same subpopulation.
The variable effects that emerge from the ATI study suggest that CMS may have missed or underestimated the impact of the risk adjustment model changes on the most vulnerable Medicare beneficiaries who suffer from the chronic conditions that affect these groups disproportionately. For example, it is well known that Black non- Hispanic populations have higher rates of both diagnosed and undiagnosed diabetes and pre-diabetes than White populations.1 It stands to reason that MA enrollees in the same demographic group, and with the same underlying conditions, may be negatively affected by CMS’s proposed risk adjustment model changes as well. The result of these changes could be a perverse incentive for MA plans to select enrollees with conditions with increased risk scores and avoid people with eliminated or decreased risk scores.
In addition to concerns about the impact of coding changes on demographic subpopulations, the ATI analysis suggests that there may be an as-yet unexplored disproportionate impact on primary care versus specialty care. As table 3 below indicates, for a significant number of codes that have been decreased in weight or eliminated in CMS’s proposed changes, there is likely to be a major impact in terms of primary care visits in which diagnoses would have been coded in these categories. The result will be that primary care practices will in effect be paid less for treating these patients, even though the evidence shows that many of these conditions can be well managed through primary care.2 This potential raises significant concern that primary care providers’ ability to screen and treat chronic conditions could be eroded, with ultimately negative effects on health outcomes, resource utilization, and costs. For example, the US Preventive Services Task Force recommends depression screening for the entire adult population, including older adults, but if primary care practices with MA enrollees lack adequate financial incentives to screen and treat depression, it is unlikely that this recommendation will be fully carried out.
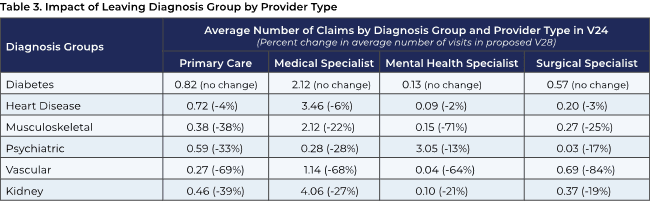 Note: Among beneficiaries who are part of the diagnosis group, average number of claims with an HCC score in that diagnosis group by provider types.
Note: Among beneficiaries who are part of the diagnosis group, average number of claims with an HCC score in that diagnosis group by provider types.
Source: ATI Advisory analysis of 2018–2020 Medicare Current Beneficiary Survey (MCBS) data
B. Analyses of APG Member Groups
Based on studies that APG, members, and others have completed, the impact of CMS’s proposed changes will be variable across APG groups. Some of our groups have advised us that the revenue decreases that they anticipate from the risk-adjustment model changes would be roughly in line with the CMS estimated average impact of –3.12 percent, or slightly better. However, other groups forecast sharply more negative effects. They have reported to us that these negative results relate to roughly 20 specific codes that they use regularly in diagnosing their patients, as the table below compiled by one APG member organization indicates.
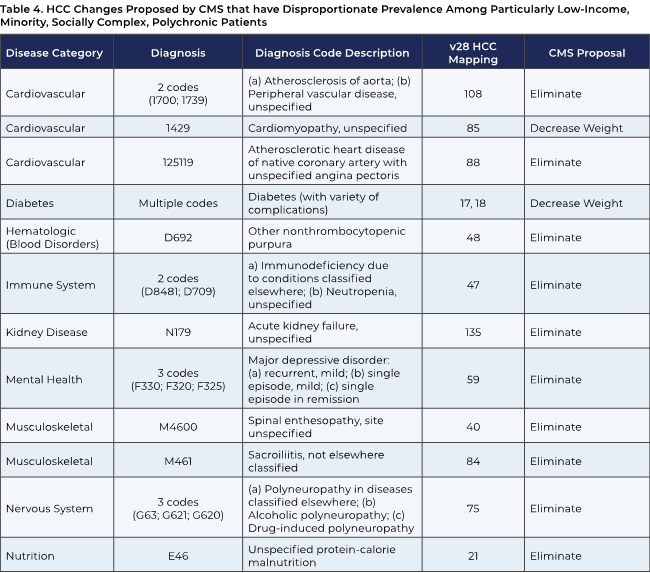
APG acknowledges that there is disagreement within the clinical community as to the advisability of carrying out some clinical interventions that are frequently coded in a limited number of the categories listed above – for example, screening for peripheral artery disease in non-symptomatic patients.4 It is also appropriate to remove any codes that reflect low-value care, both to protect patients and to enhance the integrity of the Medicare program and save money for the Trust Funds.
These exceptions aside, however, elimination or decreased weighting of most of these codes would have the effect of lowering payment that several APG groups use—not only to treat their disadvantaged patients for these corresponding conditions but also to address their needs in holistic ways. To put it bluntly, it costs a great deal to care for these patients and addressing their health needs—as well as their health-related social needs, such as transportation to medical appointments and nutritious food – are funded in multiple ways, and not solely through rebates channeled to MA health plans and on to providers.
The same APG group that provided the coding analysis above has also forecasted the impact of these coding changes on its revenues. The group foresees a net revenue impact of all the proposed changes in the Advance Notice of negative 17 percent (the midpoint of a confidence interval range of 14 percent to 19 percent). These estimates are [qualify as per below]. This group has clinics in multiple U.S. states in primarily urban locations, with a special focus on serving patients of low socioeconomic status, two-thirds of whom are underrepresented minorities, under global risk arrangements. The group anticipates that the resulting losses in revenue will wipe out their operating margins on many of these clinics, forcing them to close those in many areas and refocus on treating MA enrollees that are less disadvantaged; are in preferred-provider-organization model MA plans; or that are traditional Medicare beneficiaries who are better off and can afford Medicare supplemental insurance plans. The net effect would be to prompt this group to move away from the provision of value-based care and back to conventional fee-for-service.
Other APG member groups have developed comparable projections on the impact of the proposed risk adjustment model changes. For example, the analysis undertaken by one multi-city APG group shows a nearly 24 percent decrease in its raw risk score; with normalization, that would lead to a 14.6 percent drop in this group’s revenues from MA.
In addition, an APG medical group affiliated with a large West Coast academic medical center, which serves approximately 10,000 MA enrollees in multiple plans, anticipates the effects shown below of the proposed risk adjustment model changes. This organization has both fully delegated and percent-of-premium contracts with MA health plans.
Another APG member physician group, affiliated with a large multistate West Coast health care system, foresees a negative 12.7 percent impact on MA revenue in 2024 from the risk adjustment changes and describes the project $92 million in losses as “potentially devastating.” Underscoring the variable impact of the proposed changes, other small MA health plans affiliated with this organization that operate in different, less mature markets foresee an impact that is slightly positive.
The bottom line of these analyses is that, if CMS’s risk model revisions are finalized as proposed, beneficiaries’ access to care will be significantly disrupted as soon as January 1, 2024. As the analyses provided above, as well as other analyses, have shown, the impact will be greatest on health plans that care for the oldest and sickest populations, including those enrolled in Special Needs Plans, as well as dual-eligible enrollees and others who are frequently cared for by APG members.5
Discussions with APG members and the MA plans with which they are contracted indicate that the plans are likely to reduce or eliminate benefits, including supplemental benefits, and increase premiums and cost- sharing. Many of the benefits that will be cut, such as transportation and meals, help to support physicians’ management of people’s chronic conditions. MA plans are also likely to reduce payments to contracted physician groups.
In theory, MA plans could adjust payment terms in contracts so that the effects of the risk model revision were evenly shared by all contracted providers, but there is no requirement that they do so. CMS has historically chosen a stance of non-interference in contract terms between MA plans and providers, and the agency has not indicated any plans in the Advance Notice to deviate from this practice. What’s more, even if contract terms could be adjusted, it would be done with a considerable time lag in many instances, as some APG groups have signed contracts with MA plans as long as five years’ duration. APG groups also reject the notion – based on experience – that MA plans can or will manage their medical loss ratios in such a way as to maintain existing payment levels to providers.
Many APG member groups – those in delegated relationships with MA plans in particular – have an extreme sense of urgency to address their concerns about CMS’s proposed changes. Some note that if CMS’s proposal is finalized, these value-based care contracts with MA plans will become untenable for them. They foresee abandoning value-based care and their mission to serve disadvantaged beneficiaries, returning to FFS, and closing clinics in underserved rural areas and inner cities where affected conditions are most common as the only viable options available. With an estimated 38 percent of all licensed male physicians and 18 percent of all licensed female physicians, age 60 and older as of 2020, many APG groups predict that older physicians will simply elect to leave medical practice or retire amid disillusionment over the diminution of the ability to adequately serve patients through value-based care.6
These APG member groups stress that CMS must understand the perilous condition in which they will be left if the proposed risk adjustment model changes are finalized. One APG member group described a clinic that it operates in a major West Coast city whose ability to serve patients would only be further compromised by the proposed changes in MA:
The clinic serves many Medicaid, MA, dual eligibles, and some patients with employer-sponsored coverage. [Our] medical group is committed to serving this wonderful yet vulnerable community. We have set health equity targets for this specific community, and other nearby communities, to reduce hypertension in the Black populations. We achieved our first-year goal and plan to expand the program to achieve similar hypertension reductions in the LatinX population. However, the economic realities we face are daunting. We have a [Medicaid] managed care full-risk agreement where we lose $1 million per month, and with a 12.7% estimated decrease in Medicare Advantage payments, our service to this vulnerable community will be placed further at risk. These proposed changes aren’t forcing us to make a decision about whether we place an ad to run during the Super Bowl. They will limit the number of people we can serve in low-income communities.
C. APG’s Recommendations to CMS
Given the severity of the impact of the proposed risk model revisions, the limited time in which CMS must consider and implement changes ahead of the April 3, 2023, final rate announcement deadline, and our uncertainty about which may prove to be an acceptable approach, APG makes a three-part recommendation in order of preference.
Recommendation #1: APG proposes that CMS postpone for one year the implementation of the proposed clinical revisions to the risk adjustment model that include changes to diagnosis codes and HCCs. Such a postponement would allow time for the agency to study the variation in impact across groups that contract with MA plans, to share more details about the proposed changes, and to solicit stakeholder input on concerns, data on real-world impacts, and ideas for potential modifications to proposed revisions.
Recommendation #2: If CMS opts not to postpone implementation of the proposed risk model revisions, then APG proposes that CMS eliminate or revise the proposed changes to the limited number of diagnoses (approximately 20) that result in the largest share of the negative impact.
Recommendation #3: If CMS rejects the first and second recommendations, then APG proposes that CMS phase in the proposed clinical revisions to the risk adjustment model over two to three years.
D. Changes in Part C Star Ratings and a “Universal Foundation” for Potential Future Quality Measures
CMS proposes changes in quality measures that are discussed at length in the Advance Notice, both in the existing Part C Star Ratings and in the context of creating a “universal foundation” to align quality measures across MA and other programs. In this section, APG first discusses the Star Ratings changes and then the proposed Universal Foundation approach.
CMS identifies specific possible future Star Ratings measures, including the following:
• Chronic Pain Assessment and Follow-up
• Cross-Cutting: Sexual Orientation and Gender Identity for HEDIS Measures
• Cross-Cutting: Identifying Chronic Conditions in HEDIS Measures
• Blood Pressure Control Measures
• Kidney Health
• Social Connection Screening and Intervention
• Broadening the Mental Health Conditions Assessed by HOS
• Measuring Access to Mental Health Care on the Medicare Health Outcomes Survey (HOS)
• Addressing Unmet Health-Related Social Needs on the HOS
Although APG applauds the general direction of these proposed additions to Star Ratings – in particular, those that would provide incentives for physicians to increase efforts to identify and manage chronic and mental health conditions, such as “Cross-cutting: identifying chronic conditions in HEDIS Measures” and “Broadening the Mental Health Conditions Assessed by HOS.”
Yet at the same time, APG notes inconsistency between some of these proposals and other aspects of the Advance notice. As discussed at length above, CMS proposes changes in the risk adjustment model that would reduce the coefficients or remove diagnoses for many mild- to moderate-stage chronic conditions. These proposed changes might suggest that CMS does not really want to know about the prevalence of these conditions across the Medicare Advantage population or is not interested in having physicians diagnose and manage these conditions at early stages. CMS apparently would prefer an MA payment system that implicitly encourages physicians to wait until patients’ chronic conditions advance to the most severe stages before diagnosing and treating them.
APG believes that aligning incentives in MA for clinicians to provide both primary and secondary prevention of chronic conditions, and diagnose these conditions at early stages, is best for patients, and will support primary care practices by providing appropriate resources for the care and management of these conditions. It is not rational for CMS to send mixed signals by requiring that these conditions be reported from a quality standpoint, but not necessarily be coded from a risk adjustment standpoint.
Recommendation #1: CMS should weigh carefully whether proposed risk adjustment model changes will conflict with, and even defeat, proposed Star Ratings changes. Taking further time to examine the possible interactions among these changes would be another reason to postpone adoption of the risk model changes proposed in the Advance Notice.
Turning to the Universal Foundation, CMS proposes a common set of quality measures to achieve greater consistency and reduced complexity across the Medicare program. These shared measures would be augmented with measures unique to specific elements of the program, such as ACOs. The proposed universal measures are shown in table 6 below.
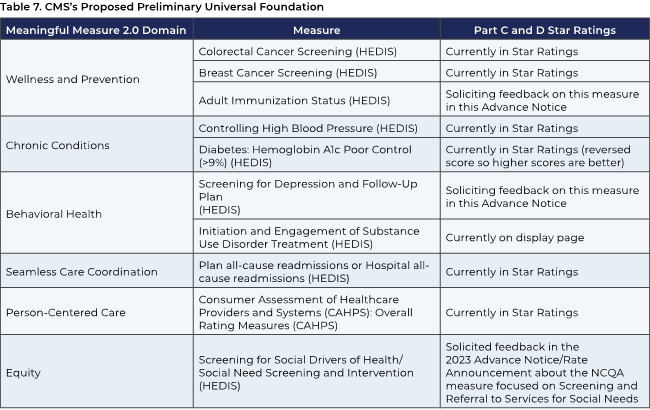
APG applauds CMS’s effort to create this Universal Foundation and greater consistency in measuring quality across Medicare. However, APG notes that both the Universal Foundation and the identified potential future Star Ratings measures still include a greater share of process measures compared to outcome measures and encourages CMS to move as expeditiously as possible to adopt more outcome measures.
In addition, APG repeats its previous recommendation that access to physicians operating in value-based care models, such as those in delegated relationships with MA plans, be added to the potential future Star Ratings measures. Such a change to Star ratings would reflect the superior quality of care that these physician groups offer, equip beneficiaries with this information to support their choice of MA plans, and help to achieve CMS’s goal of having all Medicare beneficiaries in relationships with accountable entities by 2030.
Recommendation: APG proposes that CMS include a Star Ratings measure to reward MA plans that offer beneficiaries access to physician groups that offer value-based care.
V. Conclusion
APG recognizes that CMS has full authority to make technical and even substantial changes to the risk adjustment model. However, APG requests greater transparency and time for meaningful input on revisions that constitute a policy change that fundamentally reallocates large amounts of resources without full clinical or other justification. If CMS’s proposals are finalized, MA plans and providers will adapt. But in the meantime, many beneficiaries are likely to experience dramatic changes in their access to care and benefits. The new status quo will very likely reflect a significant setback in the progress toward greater accountable care and health equity.
As noted above, it becomes increasingly apparent with time that the comparison of MA to FFS is both illogical and unsustainable as an ever-smaller share of Medicare beneficiaries remains in the FFS program each year. Currently, nearly half of all eligible Medicare beneficiaries are enrolled in MA plans. Only about a third of Medicare beneficiaries are in traditional FFS Medicare and the other two-thirds are enrolled in either MA, an ACO, or a similar program. The result of these dramatic shifts has been a sizable change in the diagnoses used for risk adjustment, Medicare spending and costs used for benchmarks, and other structural issues.
APG recognizes that CMS and others do not continue to turn to FFS as a comparator purely out of established habit or other motivation. There are no perfect alternatives that are immediately available. Determining the optimal ones will be a significant intellectual undertaking that will require time and resources. Yet time is also running short to spur the move to value, given CMS’s 2030 goal of having all Medicare beneficiaries in an accountable relationship with their health care providers.
APG urges CMS to engage with informed stakeholders, including physicians, to gather ideas for viable and equitable options, and to create a new basis for determining payments appropriate for addressing individuals’ health care needs. Such an effort would speak to the urgent realities of a world in which fee-for-service payment is a rapidly shrinking approach. It would also open a portal to a new understanding of what constitutes appropriate health care suited to the actual needs of patients, rejecting the current flawed paradigm derived from the uncoordinated, chaotic, overly costly, and frequently low-value world of fee-for-service care.
Sincerely,
Susan Dentzer
President and CEO
America’s Physician Groups
sdentzer@apg.org
1 CDC. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States. Accessed at https://www.cdc.gov/diabetes/data/statistics-report/index.html
2 Rebecca Reynolds, Sarah Dennis, Iqbal Hasan, Jan Slewa, Winnie Chen, David Tian, Sangeetha Bobba, and Nicholas Zwar, A systematic review of chronic disease management interventions in primary care. BMC Fam Pract 19, 11 (2018). https://doi.org/10.1186/s12875-017-0692-3
3 U.S. Preventive Services Task Force. Depression and Suicide Risk in Adults: Screening. Accessed at https://www.uspreventiveservicestaskforce.org/-recommendation/screening-depression-suicide-risk-adults
4 U.S. Preventive Services Task Force. July 10, 2018. Final Recommendation Statement: Peripheral Artery Disease and Cardiovascular Disease: Screening and Risk Assessment with the Ankle-Brachial Index. Accessed at https://www.uspreventiveservicestaskforce.org/uspstf/document/RecommendationStatementFinal/peripheral-artery- disease-in-adults-screening-with-the-ankle-brachial-index
5 Rob Pipich, Karin Cross, and Michael Rothschild, “High-level impacts of the proposed CMS-HCC risk score model on Medicare Advantage payments for 2024.” Accessed at https://www.milliman.com/-/media/milliman/pdfs/2023-articles/2-28- 23_2024-proposed-cms-hcc-model-impact.ashx.
6 Aaron Young, Humayun J. Chaudhry, Xiaomei Pei, Katie Arnhart, Michael Dugan, Kenneth B. Simons, “FSMB Census of Licensed Physicians in the United States, 2020.” JOURNAL of MEDICAL REGULATION VOL 107, No.2 (2021): 57.
Click here to download a copy of the letter.